 Neurobiology
Neurobiology
Innate immune memory – microglia as key players
Our study shows that the brain and its resident immune cells can acquire an immunological memory enabling the cells to either enhance or suppress their immunological response to neurological diseases, which in turn modifies disease severity. This indicates that immune memory in the brain is a previously unrecognized risk-factor for brain diseases.
Memory is the process of storing and retrieving information. In human beings, the brain is the central storage organ, and it is equipped with the neuronal system: the basis for processing memories.
But the brain is not the only place with a memory; in our bodies, many other cells are well-known for having some kind of memory. Take, for example, the cells of the adaptive immune system. These cells “remember” pathogens after their first encounter, through a process called immunological memory. Thanks to immunological memory, the immune system can adapt its response to that specific pathogen. This is the principle behind vaccination, which protects us against devastating diseases such as hepatitis.
Recent studies now also tell us that cells of the very fast reacting innate immune system, which every human is equipped with from birth, also have a kind of memory. Similar to the adaptive immune cells, innate immune cells can also adapt their immune response to pathogens that they have encountered previously. When an innate immune cell encounters a pathogen, it can lead to it reacting more strongly in a future encounter (a training effect), or to it “ignoring” the pathogen in a future encounter (a tolerance effect).
Of course, immune cells don’t have a brain to store this memory. Instead, they store this information in the packaging arrangement of their genetic code (DNA). As part of the immune response, specific regions of this code are unpacked, read and translated into proteins, which then alter the immune cell’s functions. How easily the DNA can be read depends on chemical modifications within the packaging arrangement, and altering these modifications enhances or suppresses the immune response.
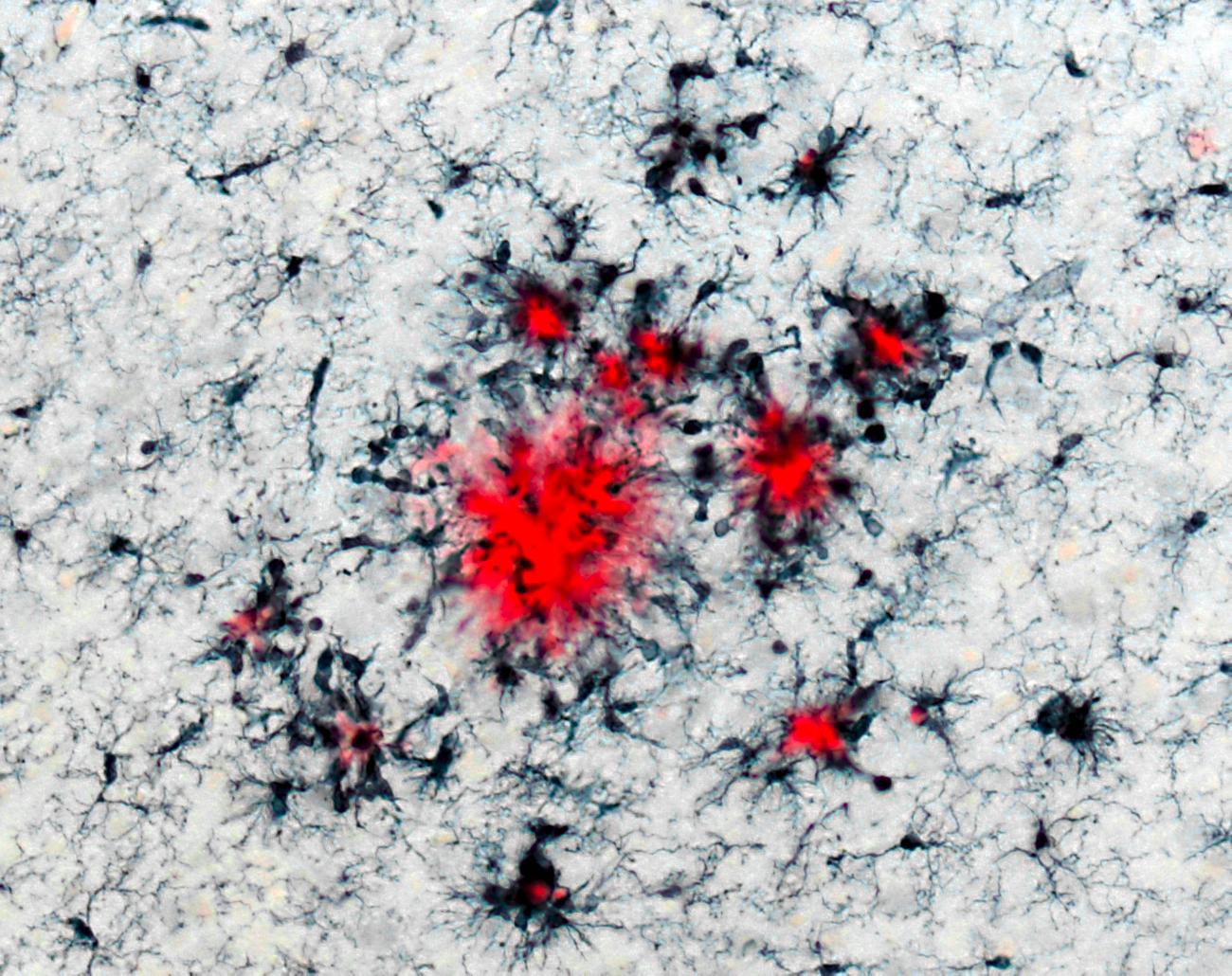
In this study we wanted to know if microglia, the brain’s immune cells, also have immune memory. Microglia are long-lived cells that are part of the innate immune system, and they are responsible for maintaining a healthy and functional brain. As such, they also play an important role in the development of brain diseases like Alzheimer’s dementia. We wondered if the immunological memory of microglia could impact the severity of symptoms of Alzheimer’s and stroke later in life. To answer this question, we used mice that are genetically modified to develop features of Alzheimer’s disease. When the mice were young, and had not developed any signs of Alzheimer’s, we injected them with a components of bacteria, which is a sure-fire way to induce a strong immune reaction. The idea was to present the mice to strong pathogen cues, see how their innate immune system (specifically, brain microglia) responded, and finally, what effect this had on the onset of their Alzheimer’s pathology. The mice received these injections daily for up to 4 days.
We found that on the first injection, brain microglia showed only a small immune reaction. However, the second injection induced a strong immune response in these cells. This meant that brain cells remembered the pathogen exposure from the first injection and, upon seeing it again, reacted strongly to combat the infection. However, on the third and fourth injection, this reaction did not occur and the initially strong immune response was shut down. It seems that brain microglia became tolerant to the infection (they began “ignoring” it). So, we were able to conclude that microglia do respond to pathogenic cues, but the number of exposures to the cue determines the reaction. After a single exposure, microglia activate their “training” program, and after three and four exposures, they activate their “tolerance” program (in this experimental setting).
How did the activation of these two different immune programs affected the onset of Alzheimer’s pathology in our mice? We found that when they received a single injection (activating the “training” program), these mice had stronger pathology of Alzheimer’s, six months later. On the other hand, when they received multiple injections (activating their “tolerance” program), Alzheimer’s pathology was alleviated!
Our results indicate that a preceding encounter of microglia with pathogens could affect the severity of neurological diseases much later in life. What does this imply for humans? Currently, it is still unclear how similar human microglia are to the microglia of a mouse. However, there is evidence for a connection between inflammation outside of the brain and neurological diseases such as Alzheimer’s in patients. These studies indicate that infections throughout life may speed up progression of Alzheimer’s disease much later, similar to the single pathogenic injection in our mice. These long-term detrimental effects in humans could indeed be mediated by immune memory in brain microglia. Thus, identifying microglia as the prominent players of innate immune memory in the brain opens up the possibility of new treatment options for neurological disease.
Original Article:
A. C. Wendeln et al., Innate immune memory in the brain shapes neurological disease hallmarks. Nature 556, 332-338 (2018)Edited by:
Dr. Carlos Javier Rivera-Rivera , Managing Editor
We thought you might like
The power of our adaptive immunity against Alzheimer’s Disease
May 10, 2017 in Health & Physiology | 3 min read by Daniele GuidoMore from Neurobiology
New, smaller-than-ever devices to help us understand how our brain works from the inside
Nov 8, 2024 in Neurobiology | 4 min read by Filippo DonatiCan we use a magnet to see brain inflammation?
Sep 25, 2023 in Neurobiology | 4 min read by Raquel Garcia-Hernandez , Santiago Canals , Silvia de SantisSurprising Behavior Changes in Genetically Modified Syrian Hamsters
Aug 30, 2023 in Neurobiology | 4 min read by Susan Lee , Kim Huhman , Jack TaylorTo achieve goals, we definitively need our neurons
Mar 10, 2023 in Neurobiology | 3.5 min read by Julien CourtinThe Impact of SARS-CoV-2 on the Brain: It Is All in Your Head
Feb 15, 2023 in Neurobiology | 3.5 min read by Meredith G. Mayer , Tracy FischerEditor's picks
Trending now
Popular topics


