 Neurobiology
Neurobiology
Can we use a magnet to see brain inflammation?
The brain's immune system helps us defend ourselves against pathogens and attacks, but what happens when it doesn't or it overreacts? Could it be dangerous? More importantly - Is there a way to detect it on time? Here we have developed a potential diagnostic tool for noninvasive detection of brain inflammation, which we believe could be critical for the diagnosis and monitoring of brain diseases.
However, what happens when this harmony is disturbed? What happens when the equilibrium is lost by an external attack or the “wear and tear” of parts? A viable system requires that balance be restored in some way. For instance, when the brain is exposed to external pathogens and/or toxins (e.g. drugs), the immune system reacts in an attempt to repel the attack and restore the equilibrium. Even the mere passing of time, e.g., non-pathological ageing, causes a sustained, low-grade activation of the immune system, termed “inflamm-ageing”.
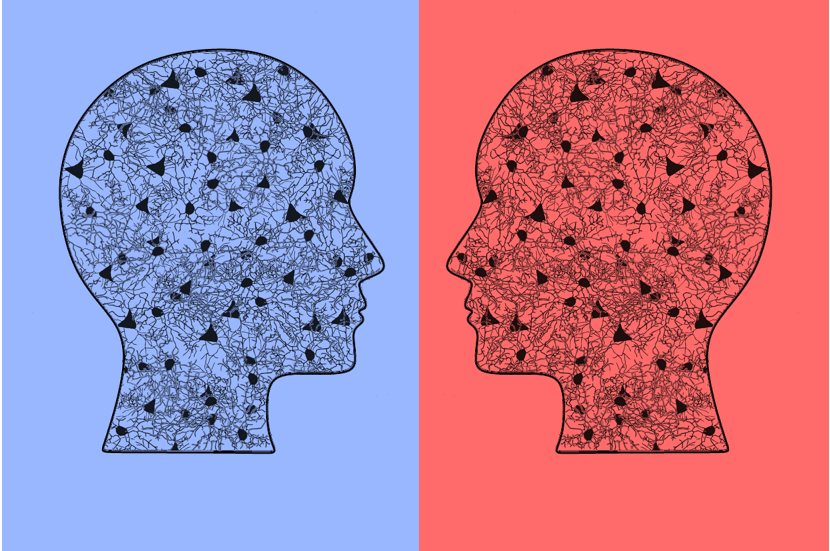
An overreaction can be quite dangerous, with outcomes such as reduced blood and oxygen flow, ischemia, and cell death. Therefore, uncontrolled neuroinflammation has functional consequences and has been linked to the progression and development of various neurodegenerative diseases such as Parkinson's, Alzheimer's and multiple sclerosis. The ability to detect early inflammatory states may offer us a source of important biomarkers for diagnosis and treatment response in neurological and psychiatric diseases. But how can we measure the tone of the neuroimmune system in vivo? The change in morphology of glial cells when confronted with a challenge can serve as a basis.
As the name suggests, diffusion magnetic resonance imaging uses the magnetic properties of water to measure how water molecules move within the brain tissue. In this work we combine this radiological technique with advanced mathematical modeling of how water navigates soft tissues to measure relevant parameters of different cell types. Our hypothesis was that by looking at water diffusing within different glial cells in different reactive conditions, we could infer their morphological changes and identify different inflammatory states.
Original Article:
Next read: The Impact of SARS-CoV-2 on the Brain: It Is All in Your Head by Meredith G. Mayer , Tracy Fischer
Edited by:
Aleksa Djorovic , Senior Scientific Editor
We thought you might like
Help or harm? How immune cells of the brain balance the immune response
Oct 7, 2020 in Neurobiology | 3.5 min read by Nathan J. Michaels , Jason R. PlemelMore from Neurobiology
New, smaller-than-ever devices to help us understand how our brain works from the inside
Nov 8, 2024 in Neurobiology | 4 min read by Filippo DonatiSurprising Behavior Changes in Genetically Modified Syrian Hamsters
Aug 30, 2023 in Neurobiology | 4 min read by Susan Lee , Kim Huhman , Jack TaylorTo achieve goals, we definitively need our neurons
Mar 10, 2023 in Neurobiology | 3.5 min read by Julien CourtinThe Impact of SARS-CoV-2 on the Brain: It Is All in Your Head
Feb 15, 2023 in Neurobiology | 3.5 min read by Meredith G. Mayer , Tracy FischerSolving A Decade-Long Mystery: Neurons Hold The Key To Rare Neurological Diseases
Feb 6, 2023 in Neurobiology | 3.5 min read by Anna-Leigh BrownEditor's picks
Trending now
Popular topics


