 Microbiology
Microbiology
What our blood can tell us about the bugs in our gut
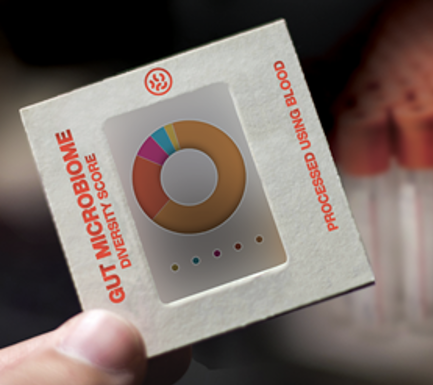
The microbes in our gut are important to our health, but we do not yet know how to tell if a particular mix of microbes is "healthy". We have found that a small group of molecules present in our blood reflects which kind of microbes live in our gut. This discovery may help in clinical practice to monitor how healthy our gut's tenants are.
We share an intimate mutual relationship with the microbes in our gut, which we call gut microbiome. It helps us digest and absorb nutrients from our food, and also support our immune system to develop and function properly. Despite considerable progress in our understanding of the human gut microbiome, we are still facing a challenge of defining how a "healthy" microbiome looks like. Abundance and presence of specific microbes can vary across different geographic locations and environments, often making translation of findings from one group of individuals to another problematic. Higher-level summary measures of the gut ecosystem have shown results that are more consistent. Generally speaking, the more bacterial species living in our guts, the better it is, while gut microbiomes comprised of fewer types of bacteria were tied to a number of diseases across populations, including recurrent Clostridium difficile infections, diabetes, and gastrointestinal disorders such as Crohn's disease.
Human blood contains thousands of different metabolites that we are now able to accurately measure at an increasingly low cost. Some metabolites come directly from our diet, others from our digestive system processing our food, and another group are the "microbial" metabolites, which are synthesized by the gut microbiome. These bacteria use the food we eat as their nourishment, and after processing it, they release metabolites into our blood. Based on this, we hypothesized that the metabolites present in our blood could reflect the composition of our microbiome. Furthermore, we believed that while gut microbes in individuals may vary across environment and geography, they might have similar effects on us.
To test our hypothesis, we used a machine learning approach. This basically means that we first uploaded blood metabolite profiles from different people into the computer and then let the computer "learn" to predict how the gut microbiome looks like for each person from the level of their blood metabolites. We then used this learned model on a new "testing" data set, and we validated how accurately it predicts gut microbiome diversity from the same blood metabolites. To our surprise, not only we were able to predict gut microbiome diversity, but the prediction relied on a small group of 40 metabolites (out of >650 we had measured). Many of the metabolites we identified were previously shown to be synthesized by bacteria in the gut. Some of these microbial metabolites were known to be associated with negative health outcomes, such as kidney dysfunction and cardiovascular disease. Another interesting finding was that blood metabolites reflect an increase or decrease in microbiome diversity under varying conditions, like antibiotics treatment or gastrointestinal disease. Moreover, we found out that these metabolites are a better predictive marker for microbiome diversity than an extensive panel of blood tests, which doctors routinely use in clinical practice to monitor the health of patients. Using our approach, we pinpointed metabolites which can be used to diagnose if a person has low, potentially problematic, diversity of bacteria living in their guts. After analyzing our results, we found that potentially toxic metabolites were associated with both low but also high diversity, suggesting that there may exist a "Goldilocks Zone", which means that neither high nor low diversity is optimal for our health.
An important implication of our work is the early diagnosis of the recurrent form of Clostridium difficile infection, which accounts for ~15,000 deaths annually in the U.S. One of the main risk factors for this bacterial infection is low gut microbial diversity, often due to use of antibiotics or other medication. A reliable clinical blood test for microbial diversity would allow us to quickly diagnose individuals at higher risk for recurrent (i.e. antibiotic-resistant) infections and perhaps employ more effective therapies, such as stool transplants from healthy donors, as a first line of treatment.
Future work is needed to untangle the complex relationship between the gut microbiome and human health. We believe that the key to defining and monitoring a healthy state of the microbiome is examining its reflection in the blood, which may be more stable, easier to measure, and universal.
Original Article:
Wilmanski T*, Rappaport N*, Earls J et al. Blood metabolome predicts gut microbiome-diversity in humans. Nat Biotechnol. 2019;37(10):1217-1228.Edited by:
Dr. Monika Stankova , Senior Scientific Editor
We thought you might like
Aquatic plants are influenced by the surrounding landscape
Aug 18, 2020 in Plant Biology | 3 min read by Ole PedersenMore than meets the eye: the histones revealed as enzymes
Jan 12, 2021 in Health & Physiology | 3 min read by Oscar A. Campos , Siavash K. KurdistaniPrickly prospects for cacti under climate change
Jun 14, 2023 in Plant Biology | 3 min read by Michiel PilletMore from Microbiology
Monoclonal antibodies that are effective against all COVID-19 -related viruses
Jan 31, 2024 in Microbiology | 3.5 min read by Wan Ni ChiaPlagued for millennia: The complex transmission and ecology of prehistoric Yersinia pestis
Jul 31, 2023 in Microbiology | 3 min read by Aida Andrades Valtueña , Gunnar U. Neumann , Alexander HerbigHow cellular transport can be explained with a flip book
Jun 5, 2023 in Microbiology | 3 min read by Christina ElsnerThe Achilles’ heel of superbugs that survive salty dry conditions
Apr 24, 2023 in Microbiology | 4 min read by Heng Keat TamNew chemistry in unusual bacteria displays drug-like activity
Mar 21, 2023 in Microbiology | 3.5 min read by Grace Dekoker , Joshua BlodgettEditor's picks
Trending now
Popular topics


