 Microbiology
Microbiology
Blocking protein folding to fight antibiotic resistance
Antibiotics are the cornerstone of modern medicine, but their effectiveness is threatened by the growing problem of antibiotic resistance. Recent research has identified a new strategy with the potential to restore the effectiveness of a range of currently used antibiotics, including drugs of last resort.
Antibiotics are medicines that prevent and cure bacterial infections. They are essential for treating a wide variety of diseases and underpin much of modern healthcare, including cancer treatment, surgery, and organ transplants.
Unfortunately, bacteria can develop the ability to survive antibiotic treatment. This is called antibiotic resistance, and it is a growing problem that could make many infections and common medical procedures much more dangerous in the near future. A landmark study from early 2022, which assessed the scale of the issue, concluded that 1.2 million people across the world died from antibiotic-resistant bacterial infections in 2019 alone.
Bacteria can become resistant to antibiotics in many different ways. One common way is the production of resistance proteins, which either break down antibiotics, or defend the part of the bacteria that the antibiotic targets. Either way, they prevent antibiotics from being effective. A tried and tested approach to overcome the problem of resistance proteins is the use of molecules called adjuvants. Adjuvants and antibiotics are mixed and given together; the adjuvant binds to the resistance protein, stopping it from working, and the antibiotic is left free to kill the bacteria. However, there are limits to this approach. Each currently used adjuvant only targets one type of resistance protein, and some resistance proteins have even evolved to break down adjuvants as well as antibiotics.
In our recent study, we asked whether we could prevent bacteria from building resistance proteins in the first place. We also wondered whether a new kind of adjuvant could work for several types of resistance protein, by blocking the assembly of these proteins, instead of just inhibiting their functions. To test these ideas, we turned to the disulfide bond formation (DSB) system, a group of bacterial proteins that help assemble a large number of other proteins in an area of the cell where many resistance proteins are found. The fact that the DSB system is not found in mammals makes it a good candidate for targeting the bacteria only, without affecting any human proteins.
With our potential “target” identified, we decided to investigate its importance for two different kinds of resistance proteins: β-lactamases and mobile colistin resistance enzymes (MCRs). β-lactamases cause resistance to β-lactam antibiotics like penicillin, the most commonly prescribed antibiotics in the world, while MCRs cause resistance to colistin, a powerful “last-resort” antibiotic used when an infection is resistant to all other available drugs.
We started by introducing the genes for 12 different β-lactamases and 5 different MCRs into two different strains of harmless laboratory Escherichia coli, one with a working DSB system, and the other without a working DSB system. Cells with a working DSB system were resistant to the antibiotics we tested, but the cells without a working DSB system were not, even though they had the genetic instructions to make the resistance proteins. When we measured how much of each resistance protein was present in the two different E. coli cells, we saw that most resistance proteins were not even made if the DSB system was not working. When a resistance protein was still being made, we measured its activity. In all cases, we found that if it had come from cells that lacked a working DSB system, it did not function properly.
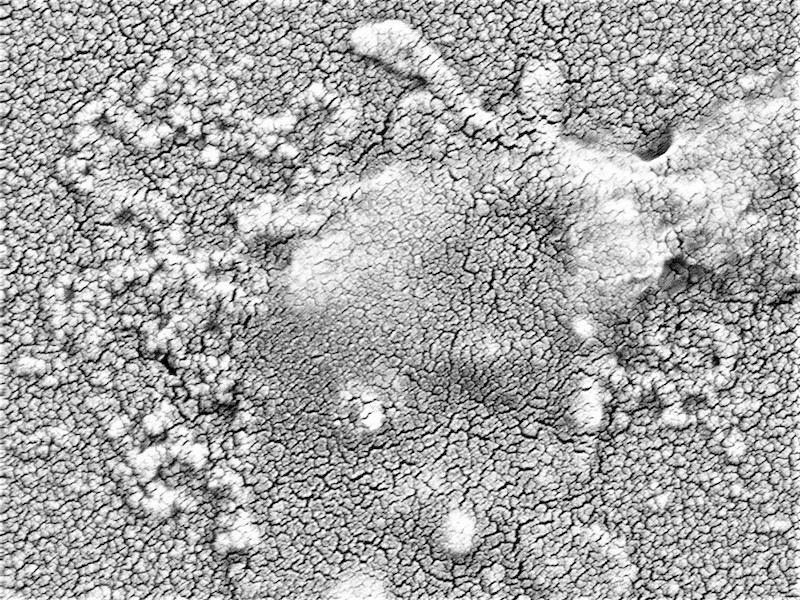
Encouraged by these results, we wanted to see whether we could use a chemical to achieve the same effect. To do this we used a small molecule found by another team of scientists that stopped the DSB system from working. When we exposed antibiotic-resistant bacteria isolated from patients to antibiotics alone, they survived, but when we exposed them to both antibiotics and the DSB system inhibitor, the previously resistant bacteria were killed. On the microscope we could even see bacteria bursting open when given the antibiotic and inhibitor combination!
Finally, we tested if our idea worked in a living organism using wax moth larvae, which are commonly used in antibiotics research. We injected two versions of an antibiotic-resistant Pseudomonas aeruginosa strain into the larvae, one with a working DSB system, and the other without. We then treated the larvae with an antibiotic. The bacteria killed the majority of the larvae in all but one case: when the P. aeruginosa without a working DSB system was treated with the antibiotic.
All of this evidence suggests that the DSB system could be a good target for a new type of antibiotic adjuvant. Clearly, much more work needs to be done, but if all goes well DSB system inhibitors could be used in the future as new, broad-acting adjuvants to help keep antibiotics working for the benefit of everyone.
Original Article:
Furniss, R. et al. Breaking antimicrobial resistance by disrupting extracytoplasmic protein folding. eLife 11, (2022).Next read: Vaccine hope against a sexually transmitted disease: the answer to the burgeoning rise in a superbug by Helen Petousis-Harris
Edited by:
Olivier Kirchhoffer , Senior Scientific Editor
We thought you might like
Fighting back antibiotic resistance: a new hope from the soil
Feb 24, 2016 in Microbiology | 4 min read by Dan KramerCollateral damage: antibiotics disrupt the balance in the gut
Jun 2, 2016 in Microbiology | 3.5 min read by Katri KorpelaInvisible allies for healthy juvenile growth
Oct 12, 2016 in Microbiology | 4 min read by Martin SchwarzerRed in Tooth and Claw: another weapon against antibiotic resistance
Oct 3, 2017 in Microbiology | 3.5 min read by Nicholas A. IsleyMore from Microbiology
Monoclonal antibodies that are effective against all COVID-19 -related viruses
Jan 31, 2024 in Microbiology | 3.5 min read by Wan Ni ChiaPlagued for millennia: The complex transmission and ecology of prehistoric Yersinia pestis
Jul 31, 2023 in Microbiology | 3 min read by Aida Andrades Valtueña , Gunnar U. Neumann , Alexander HerbigHow cellular transport can be explained with a flip book
Jun 5, 2023 in Microbiology | 3 min read by Christina ElsnerThe Achilles’ heel of superbugs that survive salty dry conditions
Apr 24, 2023 in Microbiology | 4 min read by Heng Keat TamNew chemistry in unusual bacteria displays drug-like activity
Mar 21, 2023 in Microbiology | 3.5 min read by Grace Dekoker , Joshua BlodgettEditor's picks
Trending now
Popular topics


