 Health & Physiology
Health & Physiology
Neutralizing antibodies: the Elite Squad to combat SARS-CoV-2 infection
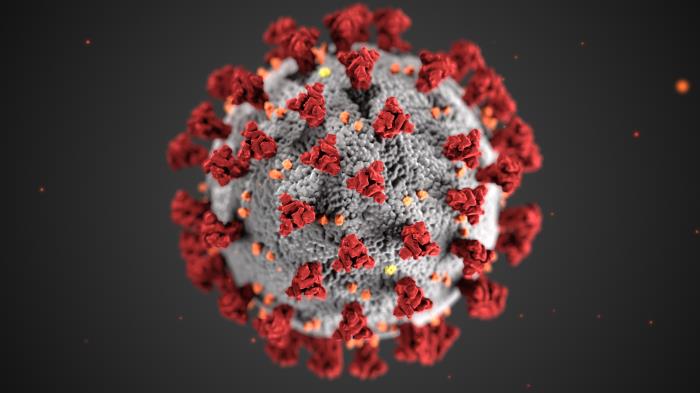
The coronavirus disease 2019 (COVID-19) pandemic caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) urgently calls for prevention and treatment interventions. Neutralizing antibodies isolated from recovered patients are capable of blocking the virus from entry into human cells, potentially acting as the “Elite Squad” to defeat SARS-CoV-2.
The rapid global transmission of SARS-CoV-2 poses a severe health emergency affecting over 20 million people worldwide as of 12 August. The research communities have taken immediate and enormous actions in search of therapeutic and prophylactic interventions. The major strategies undertaken include repurposing "old" drugs, identifying "new" drugs, and taking advantage of neutralizing antibodies produced in the plasma of survivors. Ultimately, developing vaccines that provide sufficient and long protection against infection and diseases.
Antibodies are a major component of our immune system. Secreted by B lymphocytes, antibodies are responsible for binding and eliminating pathogens through specific mechanisms. However, only a fraction of antibodies can block viruses from entering the cells. These antibodies are therefore called "neutralizing antibodies". Neutralizing antibodies hold a great promise for clinical intervention. A substantial number of investigational neutralizing antibodies are under development for diverse infectious diseases. Notably, three have received approval to prevent respiratory syncytial virus (palivizumab) and prevent and treat anthrax (raxibacumab and obiltoxaximab).
Since the outbreak of COVID-19, we have been working on how SARS-CoV-2 enters the cell, and isolating neutralizing antibodies can disrupt the entry process. Like severe acute respiratory syndrome coronavirus (SARS-CoV) identified in 2003, SARS-CoV-2 utilizes its spike glycoprotein envelope to interact with a host cellular receptor called angiotensin-converting enzyme 2 (ACE2). This receptor is highly present in vital organs, such as the lungs. Like a key opening a lock, this binding of spike with ACE2 triggers a cascade of events leading to cell membrane fusion, making a hole on the cell as a way of entering the cell. In March 2020, we and others have resolved the crystal structure of spike's receptor-binding domain (RBD) bound to ACE2. Such information is critical for our better understanding of the structural basis of spike-ACE2 interaction and providing a precise target for antibody research and development.
The article published in Nature highlighted our efforts to successfully isolate powerful neutralizing antibodies from SARS-CoV-2 infected individuals. We started by collecting blood samples from eight infected patients in Shenzhen, China. We then used spike's RBD as a bait to fish out 206 antibodies from millions of B lymphocytes in the blood. Genetic analysis of antibodies demonstrated that each patient has a unique antibody repertoire pattern in response to SARS-CoV-2. When zooming into Patient #2 for more in depth analysis, we identified three antibody clones that dramatically expanded, indicating a strong selection for these antibodies. However, the underlying selection mechanism is unknown.
Furthermore, we used both pseudovirus and live SARS-CoV-2 culture to evaluate the neutralizing activity and identified three antibodies as the most potent neutralizers. More interestingly, these antibodies compete with ACE2 to bind to RBD, suggesting they exerted neutralizing activity by disrupting ACE2 engagement. To further study the structural basis for antibody neutralization, we resolved one antibody's structure bound to SARS-CoV-2 RBD. The structure analysis at the atomic level demonstrated that when the antibody binds to RBD, it precludes the virus from engaging with its receptor, thereby blocking viral entry.
We also studied whether plasma from SARS-CoV-2 infected individuals could cross-recognize SARS-CoV spike's RBD, given their sequential and structural similarities. Unexpectedly, neither SARS-CoV-2 infected plasma nor isolated antibodies cross-reacted with SARS-CoV RBD. On the flip side, previous isolated SARS-CoV antibodies also failed to cross-neutralize SARS-CoV-2. The lack of cross-reactivity highlights that the two antibody responses are quite distinct. Specific intervention strategies have to be designed and developed for each viral species to achieve maximum efficacy.
Overall, our study has provided important insights into the antibody response elicited by SARS-CoV-2 infection. Of course, many tough questions remain. For example, whether antibody response has a direct impact on disease severity? Whether an antibody response is the cause or consequence of severe infection? Answers to these questions are critical for monitoring diseases and initiating interventions at the appropriate time to attenuate disease progression. Scientists worldwide, including our team, are actively addressing these questions. In the meantime, we have been working tirelessly to push our neutralizing antibodies into clinical development. The two most potent ones are under evaluation in Phase I clinical trial in China, in collaboration with Brii Biosciences and Beijing Ditan Hospital. More inspiringly, there have been at least five neutralizing antibodies under clinical evaluation worldwide, bringing more potential weapons to combat SARS-CoV-2.
Original Article:
Ju B, Zhang Q, Ge J, et al. Human neutralizing antibodies elicited by SARS-CoV-2 infection. Nature. 2020;584(7819):115-119.
Next read: Understanding how COVID-19 Patients shed viral particles into their environment by Joshua L. Santarpia
Edited by:
Massimo Caine , Founder and Director
We thought you might like
The Face Mask Dilemma: to wear or not to wear, that is the question
Apr 6, 2020 in Health & Physiology | 4 min read by Reinier ProseeThe evolution of the new coronavirus: what the past teaches us for a better future
Apr 9, 2020 in Evolution & Behaviour | 3.5 min read by Akira OhkuboThe importance of being tested
Jul 15, 2020 in Health & Physiology | 3.5 min read by Giulia GiordanoT cells: an essential but neglected component against COVID-19
Nov 4, 2020 in Health & Physiology | 4.5 min read by Antonio Bertoletti , Anthony Tan , Nina Le BertMore from Health & Physiology
Tobacco smoking and other exposures shut off cancer-fighting genes
Aug 31, 2024 in Health & Physiology | 3 min read by Jüri Reimand , Nina AdlerA hidden clock that times cytoplasmic divisions
Aug 30, 2024 in Health & Physiology | 3 min read by Cindy OwWhen two kinases go for a dance
Aug 2, 2024 in Health & Physiology | 4 min read by Ioannis Galdadas , Francesco Luigi Gervasio , Pauline JuyouxAwakening the thymus to cure SARS-CoV-2 infection: a matter of genes
Jul 27, 2024 in Health & Physiology | 3.5 min read by Stefano Marullo , Cheynier RemiKeeping the balance: How epigenetics monitors cancer genes
May 13, 2024 in Health & Physiology | 4 min read by Zach Gray , Madison Honer , Johnathan WhetstineEditor's picks
Trending now
Popular topics


