 Health & Physiology
Health & Physiology
De-liver-ing blood and immune cells to the developing human
Little is known about how the human immune system develops before birth. However, with advances in sampling methods and gene mapping technologies, we have completed an atlas of the developing blood and immune systems. This will enable us to use this knowledge for tissue engineering and regenerative medicine and to better understand diseases.
Some blood and immune disorders have origins during early human development. To treat these diseases effectively, we must understand what is occurring during normal development and how critical changes in cellular expansion could lead to disease.
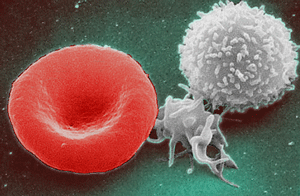
In adulthood, our blood and immune cells are made in the bone marrow. However, the bone marrow is not formed until the 12th week of pregnancy. Before this time, the liver is the leading site of blood and immune cell production. The liver is a large organ at this stage. Over gestation, the cellular composition and organisation of the tissue can change significantly. Until now, we have never fully understood these changes. In a world-first, we have created a complete cell "atlas" of the liver during the first and second trimesters of pregnancy, describing the cellular landscape of the developing blood and immune systems.
We created the atlas using a newly established technique called single-cell RNA sequencing. The method allows us to study cells individually, providing insights into their function. Traditional methods make it much more challenging to do this as they involve measuring populations of cells or whole tissue. Single-cell RNA sequencing has facilitated the discovery of new cell populations and functions. We combined this technique with methods that allow us to locate these cells within tissues, building a complete picture. Validating our findings was also an essential aspect of the study so we could confirm our observations using different experimental modalities.
The atlas revealed how different cell types change in frequency over gestation. In early pregnancy, there were many more blood cells, whereas later on, immune cells dominated. We believe this is due to the changing demands during human development. The first challenge is to establish a blood system so oxygen can circulate in the body. Once this has been achieved, the immune system arises, in preparation for any potential contact with pathogens. We designed an experiment to find out if the stem cells in the developing liver generated different types of blood and immune cells by gestation. Stem cells from the youngest and oldest prenatal liver were cultured in the laboratory to evaluate the cell types they differentiated into. Strikingly, we observed the same proportion of blood and immune cells in the petri dish as we had seen in the liver tissue. The younger stem cells formed more blood and the older stem cells made more immune cells. This suggested that the stem cell potential is due to an innate property of the cells. Remarkably, we observed mature and immature blood cells in the early developing skin, suggesting additional sites for blood formation. This capability is lost in adults but demonstrates how oxygen-carrying red blood cells are so vital to survival in early life. The immune cells we detected were captured migrating to other tissues and becoming more specialised as they matured, by gaining features specific to the tissues they inhabited.
We felt it was important that all data from the study was made publicly available. We have provided the data freely through a user-friendly interactive portal. This enables everyone to browse the data, explore genes they are interested in and investigate the expression of these genes in the cells within the developing liver. The essential conclusions from this study provide a comprehensive resource for understanding prenatal human development. Further work could involve looking at specific cells and genes related to diseases, thus widening our knowledge of disease and supporting the advancement of new treatments.
Discoveries like this are becoming more frequent through the Human Cell Atlas (HCA) initiative. This is a global community effort by scientists all around the world to map every cell in the human body. The blood and immune development study is analogous to mapping one tiny country in the complete atlas and will contribute to the mission of fully understanding human health and disease.
Original Article:
Popescu D, Botting R, Stephenson E et al. Decoding human fetal liver haematopoiesis. Nature. 2019;574(7778):365-371.Next read: Carnivorous plants help uncover universal rules of plant development by Beatriz Gonçalves , Christopher Whitewoods
Edited by:
Massimo Caine , Founder and Director
We thought you might like
A new way to go gray
Nov 23, 2018 in Health & Physiology | 3.5 min read by Christopher R. Keys , Melissa HarrisBlood-eating cells: a defense or a threat?
Aug 21, 2019 in Health & Physiology | 4 min read by Holly Akilesh , Hayley Waterman , Jessica HamermanPowering up the emergency response to infections
Jun 4, 2020 in Health & Physiology | 3 min read by Jayna J. Mistry , Kristian M. Bowles , Stuart A. RushworthMore from Health & Physiology
How obesity can improve the efficacy of cancer treatment: role of the sex hormone estrogens.
Dec 3, 2025 in Health & Physiology | 3.5 min read by Eloïse Dupuychaffray , Carole BourquinTobacco smoking and other exposures shut off cancer-fighting genes
Aug 31, 2024 in Health & Physiology | 3 min read by Jüri Reimand , Nina AdlerA hidden clock that times cytoplasmic divisions
Aug 30, 2024 in Health & Physiology | 3 min read by Cindy OwWhen two kinases go for a dance
Aug 2, 2024 in Health & Physiology | 4 min read by Ioannis Galdadas , Francesco Luigi Gervasio , Pauline JuyouxAwakening the thymus to cure SARS-CoV-2 infection: a matter of genes
Jul 27, 2024 in Health & Physiology | 3.5 min read by Stefano Marullo , Cheynier RemiEditor's picks
Trending now
Popular topics


