 Health & Physiology
Health & Physiology
Blood-eating cells: a defense or a threat?
Anemia may be caused by alterations in red blood cell development or destruction. We identified an immune cell that develops during inflammation or infection that eats red blood cells, leading to severe anemia. We propose these cells may be beneficial in fighting bacterial or parasitic infections.
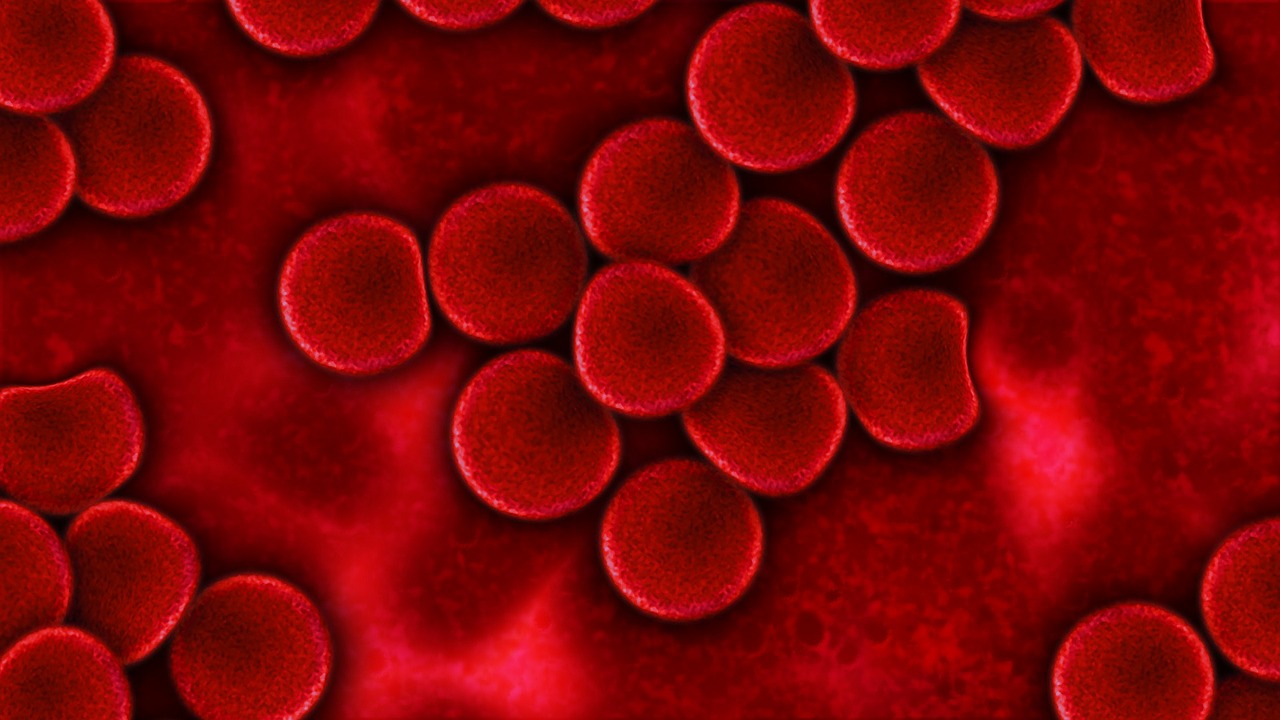
Anemia, a term you may have come across in an internet search or while donating blood at your local blood bank, is a condition in which you don't have enough healthy red blood cells. Red blood cells are important to deliver oxygen to your body, therefore, the lack of them represents a serious medical condition. There are two main ways in which you can become anemic: either not enough red blood cells are being made or they are being destroyed faster than they can be made. In some cases, anemia can be caused by chronic inflammatory diseases or infection. Inflammation is the general term for your immune system switching to a more active state and is important for clearing infections, but chronic inflammation can be detrimental to your health. Recent research from our lab highlights the importance of this balance between beneficial and harmful inflammation in a newly discovered cause of anemia.
Our lab is interested in how inflammation can influence immune cells. Through this research, we discovered a new mechanism that can lead to severe anemia in a disease called Macrophage Activation Syndrome. The macrophage is a type of immune cell that protects you from harmful invading pathogens by eating and digesting pathogens. The increased inflammation during infection or chronic inflammatory diseases can alter the function of macrophages so they become more aggressive and indiscriminate during their "cleanup" efforts, leading to diseases like Macrophage Activation Syndrome. MAS is a particularly acute and life-threatening inflammatory condition that can accompany rheumatic disease in which activated macrophages found in the bone marrow, spleen, and liver, seek and destroy red blood cells (together with other types of cells), critically reducing their numbers and leading to anemia.
One of the ways macrophages respond to infection is through receptors called Toll-like receptors or TLRs. One of these receptors, called TLR7, is located inside of macrophages, which use it to know when they have consumed a pathogen worth responding to. The role of TLR7 is similar to that of an alarm - it alerts the cell to the presence of potential pathogens. This stimulates the clearing of the infection and, in turn, it reinforces the inflammation. We have previously shown that when the TLR7-alarm is activated, macrophages develop a particular specialization, important to address the infection. This led us to wonder, "What type of macrophage develops during the TLR7 alarm?".
To answer this question, we used published data that categorizes the identity and function of macrophages in different situations to help define the type of macrophages that develop during the TLR7 alarm. We found that the macrophages that develop during the TLR7 alarm were similar to cells specialized to eat red blood cells found in the spleen, an immune organ.
We then wanted to know what might happen inside an organism when TLR7 is excessively stimulated (for example, during chronic inflammation). To answer this question, we looked at the macrophages in mice engineered to have excessive TLR7 signals. Interestingly, we found that these engineered mice had a unique type of macrophage that had eaten large numbers of red blood cells. These engineered mice were also severely anemic. We dubbed these new macrophages "inflammatory hemophagocytes", or iHPCs. In subsequent experiments, we found that these cells were responsible for the severe anemia in the engineered mice. Furthermore, we determined that these engineered mice can be a model for Macrophage Activation Syndrome. This work led us to ask about other conditions where infection can lead to severe anemia, such as during malaria in young children. We found that iHPCs were directly correlated with malarial anemia.
In conclusion, we have identified a new cell type, the "inflammatory hemophagocyte", which voraciously consumes red blood cells. This cell type develops through signals that are sensed by TLRs during both infection and autoimmunity. We believe that Macrophage Activation Syndrome may be caused by iHPCs and that these cells also cause severe malarial anemia.
So why has this immune cell type, the iHPC, evolved if it can be detrimental to the host by causing severe anemia? Maybe iHPCs evolved to eat and kill malaria infected red blood cells as red blood cells are the principal reservoir of the Plasmodium parasite during malaria infection. Alternatively, iHPCs may help slow the growth of bacteria that infect you right after a viral infection. Some of these bacteria use iron from red blood cells to grow. In these ways, anemia may be beneficial during infections. Future studies in our lab aim to determine if this is the case and why iHPCs are overactive during Macrophage Activation Syndrome.
Original Article:
H. M. Akilesh et al., Chronic TLR7 and TLR9 signaling drives anemia via differentiation of specialized hemophagocytes. Science 363, (2019)Edited by:
Massimo Caine , Founder and Director
We thought you might like
Virus infection: may the (binding) force be with you?
Jan 11, 2019 in Microbiology | 4 min read by Martin Delguste , David AlsteensPowering up the emergency response to infections
Jun 4, 2020 in Health & Physiology | 3 min read by Jayna J. Mistry , Kristian M. Bowles , Stuart A. RushworthIs 37.0 °C still a normal body temperature?
Apr 1, 2021 in Health & Physiology | 3.5 min read by Margaux HéritierCOVID-19 during pregnancy causes fetal and placental inflammation
Jul 28, 2022 in Health & Physiology | 3.5 min read by Derek Miller , Valeria Garcia-Flores , Nardhy Gomez-LopezMore from Health & Physiology
Tobacco smoking and other exposures shut off cancer-fighting genes
Aug 31, 2024 in Health & Physiology | 3 min read by Jüri Reimand , Nina AdlerA hidden clock that times cytoplasmic divisions
Aug 30, 2024 in Health & Physiology | 3 min read by Cindy OwWhen two kinases go for a dance
Aug 2, 2024 in Health & Physiology | 4 min read by Ioannis Galdadas , Francesco Luigi Gervasio , Pauline JuyouxAwakening the thymus to cure SARS-CoV-2 infection: a matter of genes
Jul 27, 2024 in Health & Physiology | 3.5 min read by Stefano Marullo , Cheynier RemiKeeping the balance: How epigenetics monitors cancer genes
May 13, 2024 in Health & Physiology | 4 min read by Zach Gray , Madison Honer , Johnathan WhetstineEditor's picks
Trending now
Popular topics


