 Health & Physiology
Health & Physiology
Can nerve signals put a halt to type 1 diabetes?
In type 1 diabetes the immune system attacks cells in the pancreas, causing chronic problems with blood sugar. It has long been a mystery why the immune system does these attacks. We discovered that nerve cells may play an important role, and this could be an important step in finding a treatment.
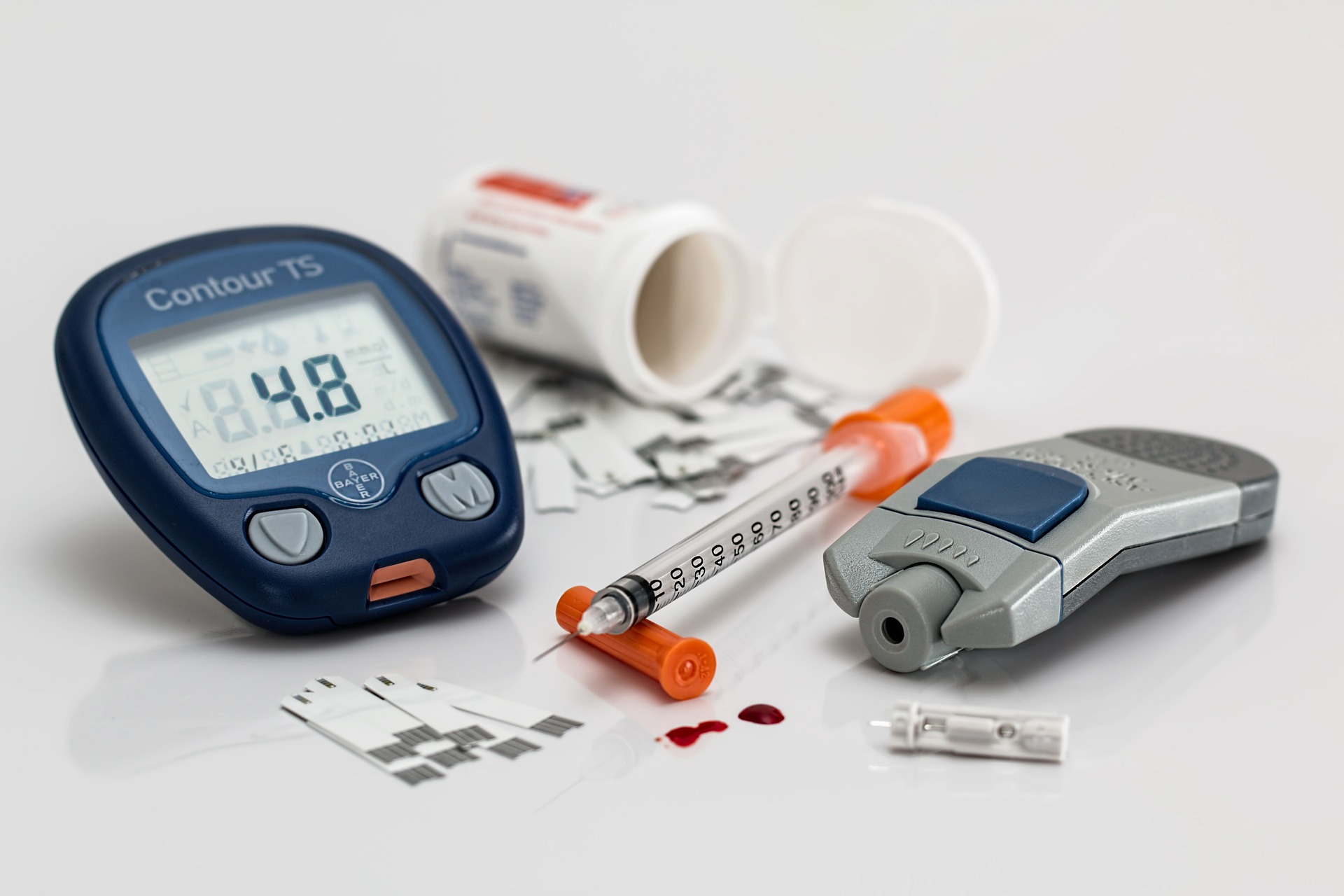
In type 1 diabetes the immune system goes awry, but the reasons why are not completely understood, and we lack treatments to control type 1 diabetes. We found that nerve signals may hold one key to solving the mystery. Normally your blood sugar level is controlled by insulin, which is produced by so-called ‘beta cells’ in the pancreas. However, for people with type 1 diabetes this is different – for unknown reasons, the body’s immune system attacks the beta cells. This means the body is not able to produce enough insulin, causing high blood sugar levels and a myriad of health problems as a result. Unfortunately, nobody knows what triggers the immune system to attack beta cells. Decades of research have found several culprits and potential suppressors among our immune cells, but the full picture is still not clear.
In a search for mechanisms behind this disease, we looked at the pattern of beta cell destruction in the pancreas. This pattern has been known for long to be ‘patchy’, where beta cells in certain areas of the pancreas are killed off whereas other areas seem to remain untouched. We think that an explanation for this pattern could lie in where nerves are located the pancreas.
We set out to test whether nerves could explain parts of this. There is no way to study this in humans with type 1 diabetes. To cause a condition similar to type 1 diabetes in experimental animals, we used mice that have genetically altered beta cells. In the right conditions, the immune system will then recognize and attack the altered beta cells. While not a perfect analogue, this does mimic type 1 diabetes in humans, and is in line with how we think the disease works.
We then removed nerves from the mouse’s pancreas, either through surgery or using drugs. We found that blocking nerve signals to the pancreas reduced the killing activities of the immune cells, and left the beta cells unharmed. When we imaged the live beta cells in three dimensions, we made surprising observations. Watching the immune cells migrate in the pancreas, we could see that in mice where we removed the nerves in the pancreas, the immune cells that would normally attack the beta cells seemed instead uninterested in their usual targets and spared them, resulting in mice that did not develop type 1 diabetes.
To understand why the immune cells acted this way in absence of nerve signals, we investigated if immune cells located at the beta cells were able to receive nerve signals. We found that one type of immune cell, the macrophage, had receptors for adrenaline and noradrenaline – important ‘messenger’ substances released by certain types of neurons. If we then added these substances to the macrophages, they responded by either becoming more or less active, depending on the amount of substance given. These cells may be a particularly important gatekeeper at the beta cells, because when we completely removed macrophages from mice, they did not get diabetes.
We hope that our observations can help develop a treatment for type 1 diabetes. If our nervous system has a strong effect on immune cells, then interfering with nerve signals might be a viable way to dampen the response against the beta cells. If we can observe these effects also in humans, then treatments could include removing nerves in the pancreas, electrostimulation of nerves, or drugs to block nerve signals.
We knew that the immune response in type 1 diabetes is complex, and the ongoing untangling of this has been ongoing for decades. Now, we introduce nerves as yet another player, but even if it adds complexity to the game, it also adds more targets to use in future treatments of a disease that currently lacks them.
Original Article:
Christoffersson, G., Ratliff, S. & von Herrath, M. Interference with pancreatic sympathetic signaling halts the onset of diabetes in mice. Science Advances 6, (2020).Next read: Engineered probiotic boosts cancer therapy by Yonika Larasati
Edited by:
Dr. Rik Voorhaar , Senior Scientific Editor
We thought you might like
Tumor infiltrating immune cells predict patient outcomes
Oct 14, 2020 in Health & Physiology | 3 min read by Caroline S. Jansen , Haydn T. KissickCharting the immune landscape in brain cancers
Nov 27, 2020 in Health & Physiology | 4 min read by Klara Soukup , Johanna A. JoyceHow do immune cells enter tissues to protect the body?
Jan 17, 2023 in Health & Physiology | 3.5 min read by Daria Siekhaus , Maria AkhmanovaMore from Health & Physiology
Tobacco smoking and other exposures shut off cancer-fighting genes
Aug 31, 2024 in Health & Physiology | 3 min read by Jüri Reimand , Nina AdlerA hidden clock that times cytoplasmic divisions
Aug 30, 2024 in Health & Physiology | 3 min read by Cindy OwWhen two kinases go for a dance
Aug 2, 2024 in Health & Physiology | 4 min read by Ioannis Galdadas , Francesco Luigi Gervasio , Pauline JuyouxAwakening the thymus to cure SARS-CoV-2 infection: a matter of genes
Jul 27, 2024 in Health & Physiology | 3.5 min read by Stefano Marullo , Cheynier RemiKeeping the balance: How epigenetics monitors cancer genes
May 13, 2024 in Health & Physiology | 4 min read by Zach Gray , Madison Honer , Johnathan WhetstineEditor's picks
Trending now
Popular topics


