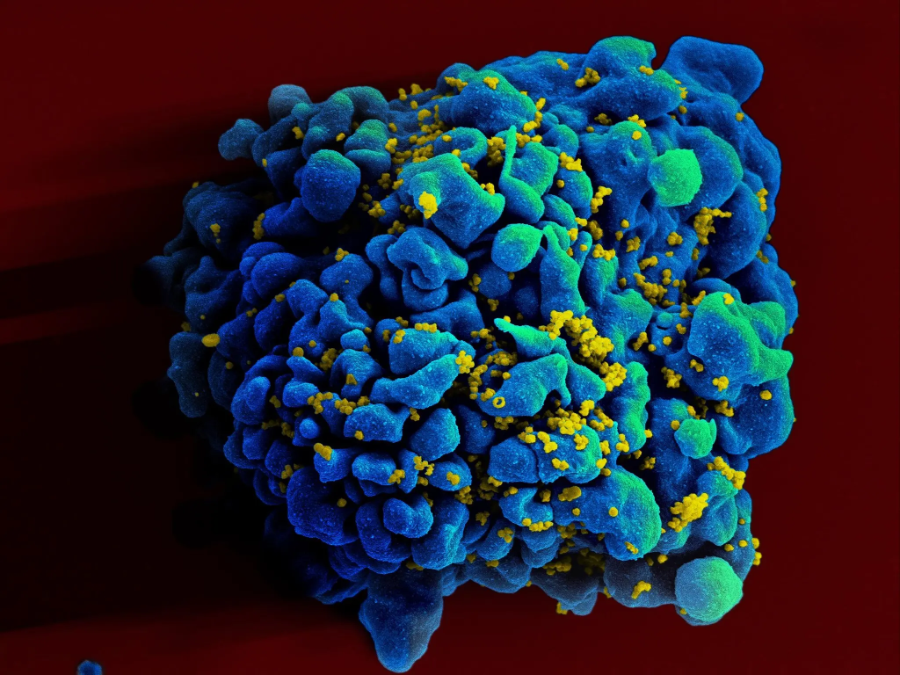
The human immune system is very effective in eliminating pathogens that attack us in everyday life. However, in the case of HIV infection, it fails to clear all infected cells, resulting in a disease that remains incurable to date. Our study reveals that HIV-infected cells express higher levels of immune checkpoint markers and 'do not kill me' signals, helping them evade immune detection.
Views 2012
Reading time 4 min
published on Sep 27, 2023
About 38 million people live with Human Immunodeficiency Virus (HIV) worldwide and hopes for a significant reduction of new transmissions have only partially materialized. In contrast to other infectious diseases that can be readily cured with short-term antimicrobial treatment, HIV-1 infection remains incurable and requires continuous suppressive treatment. Indeed, once HIV treatment is stopped, viral rebound occurs almost always within a few weeks.
The reason for this failure is the ability of HIV-1 to persist in specific cells, frequently called HIV reservoir cells, where HIV genetic material is integrated into host genes and becomes a part of the cell's own genetic material. The persistence of these reservoir cells is a major obstacle to curing HIV, as they can reactivate and produce new viruses if the treatment is stopped, thus making ART a required life-long commitment at present. Furthermore, HIV-1 can adopt a state where the virus is present in the body but remains almost inactive, a concept called “latency”, making it difficult for the immune system to detect and eliminate the infected cells. As a result, the frequency of HIV-1 reservoir cells declines very slowly over time after ART initiation.
Most of the viral DNA integrated into the host genome bears mutations and/or deletions, only a small portion of the infected cell harbors genome-intact proviruses, that are potentially able to produce new viruses after activation. The frequency of HIV-1 reservoir cells harboring intact genome declines faster than those harboring a defective genome after ART initiation, which suggests that cells harboring intact HIV-1 are more vulnerable to host immune effects.
How can the latently infected cells persist during all these years and resist immune-mediated elimination? This question is now front and center in HIV research and may offer important clues for finding a cure for HIV. However, studying these cells has been extremely difficult, predominantly because their frequency in humans is extremely low; typically, only 1 out 10,000 to 100,000 CD4 T cells in people living with HIV encodes for intact HIV. To analyze these very rare cells, Sun et al. developed a new technique called ‘Phenotypic and Proviral Sequencing’ (PheP-seq) which allows, at a single cell level, to distinguish between cells harboring no viral DNA, defective or intact viral DNA, and to study the surface proteins of these rare cells, which can influence how the immune system interacts with them.
Two findings of these studies are particularly notable: First, cells harboring intact HIV frequently express higher levels of so-called immune checkpoint markers. These molecules reduce cell activation and have also been shown to limit a cell’s ability to express HIV genes. This could help these cells to slip under immunological surveillance and translates into a higher likelihood of remaining invisible to the immune system. In addition, the infected cells harboring intact proviruses also expressed higher levels of molecules that communicate a “do not kill me” message to immune effector cells. Overall, the expression of both “immune-checkpoint” molecules and molecules communicating a “do not kill me” message to the immune system may contribute to the ability of HIV reservoir cells to persist lifelong and avoid elimination by human immune responses. These findings suggest that by manipulating these molecules, we might be able to make these cells visible to the immune system, opening new avenues for HIV treatment.
Interestingly, the mechanisms involved in the persistence of HIV-1-infected cells seem to be different in lymphoid tissues. In contrast to infected cells from the blood, as described above, the infected cells from the lymph nodes show phenotypic features associated with survival and resistance to apoptosis (a type of cell death), likely promoting their long-term persistence. This difference highlights the complexity of HIV's evasion strategies and suggests that a successful treatment approach may need to consider the unique characteristics of different tissues.
This study suggests that HIV reservoir cells, particularly those harboring intact proviruses, are under some form of attack from the human immune system. It appears that only a small subset of reservoir cells that express specific surface markers allowing them to resist host immunity can survive and persist long-term. This work offers hope that ultimately, it will be possible to tailor immune responses so that they can overcome these resistance mechanisms and be more effective in clearing all HIV-infected cells from the human body. By better understanding these resistance mechanisms, we move one step closer to developing treatments that could potentially eradicate HIV from the body.
Original Article:
Sun, W., Gao, C., Hartana, C.A. et al. Phenotypic signatures of immune selection in HIV-1 reservoir cells. Nature 614, 309–317 (2023). https://doi.org/10.1038/s41586-022-05538-8
 Health & Physiology
Health & Physiology