One of the major challenges in cancer therapy is the recurrent emergence of resistance. In pancreatic cancer, we uncovered one such resistance mechanism. Inhibiting a protein which is highly expressed in a therapy-resistant subtype of pancreatic cancer could pave the way for new therapies and improve survival of patients.
Views 2282
Reading time 4 min
published on Mar 13, 2023
The pancreas has two main functions: 1) it regulates blood glucose levels by producing insulin and glucagon and 2) it produces digestive enzymes to allow us to utilize the food we eat. Every day, up to two liters of digestive juice are passed into the small intestine via the pancreatic duct, which runs through the entire pancreas.
Up to 95% of all pancreatic cancers originate from cells located in the pancreatic duct. Because pancreatic cancer initially causes few symptoms, it is often diagnosed at a late stage. By then it is usually too late for a surgical cure and patients are treated with harsh chemotherapy. Although chemotherapy is aggressive, few patients respond effectively to it. Therefore, it is necessary to develop new treatment options and improve patient survival.
Pancreatic cancer is not a single disease, but is divided into different subtypes. One approach that allowed cancer researchers to discover several subtypes was the analysis of specific intracellular programs that can activate groups of genes and thus mediate their transcription into readable blueprints (the so-called messenger RNA, or mRNA for short). As a reminder, genes are encoded on DNA, then mRNA is transcribed from DNA and from this the protein is translated, which is ultimately required for the biological process. By analyzing the intracellular transcription programs in pancreatic cancers, various studies have consistently identified a particularly aggressive subtype. Interestingly, this aggressive subtype is characterized by a high amount of mRNA of a protein that should drive the cell into programmed cell death.
But why is there so much of one mRNA or its protein and if the protein should kill cells, why does the cancer cell not die? In addition to the cell death-promoting proteins, there are some proteins that guarantee cell survival and antagonize these cell death-promoting proteins. These cell survival proteins are also particularly highly expressed in the cancer cell. MCL1 is such a protein that ensures cell survival and prevents cell death. On the other hand, NOXA can neutralize MCL1 and make the pancreatic cancer cell ready to die. The balance of these proteins, among others, determines whether the cell is directed to survive or to die. If there is already a lot of a cell death-promoting protein, just a little more of it is needed to tip the balance and cell death is initiated. The straw that breaks the camel's back, so to speak.
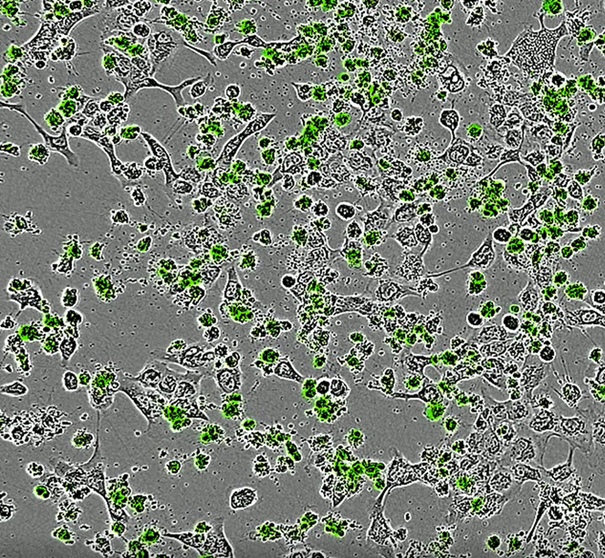
To see how we could find this extra straw, we screened almost 2000 substances and were able to identify one substance that worked, killing the cancer cells. We were initially puzzled by the mode of action of this substance, as it inhibits a factor called RUNX1 that has not been previously assigned an important role in pancreatic cancer but has been in other cancers. RUNX1 is a transcription factor, meaning it regulates (promotes or prevents) the transcription of DNA into mRNA.
We found that there are significantly higher levels of RUNX1 in pancreatic cancer compared to normal pancreas. We showed that inhibiting RUNX1 can initiate cell death in an aggressive subtype of pancreatic cancer. Therefore, in this pancreatic cancer subtype, inhibiting RUNX1 gives the extra boost to make more NOXA protein, which breaks the camel’s back, triggering cancer cell death.
Further development of a potential RUNX1 inhibitor-based therapy for pancreatic cancer will show whether our very promising data will lead to an improvement in the clinical situation.
Original Article:
Doffo, J., Bamopoulos, S. A., Köse, H., Orben, F., Zang, C., Pons, M., den Dekker, A. T., Brouwer, R. W. W., Baluapuri, A., Habringer, S., Reichert, M., Illendula, A., Krämer, O. H., Schick, M., Wolf, E., van IJcken, W. F. J., Esposito, I., Keller, U., Schneider, G., & Wirth, M. (2022). NOXA expression drives synthetic lethality to RUNX1 inhibition in pancreatic cancer. Proceedings of the National Academy of Sciences, 119(9). https://doi.org/10.1073/pnas.2105691119
 Health & Physiology
Health & Physiology